A Feasibility of Useful Cell-Based Therapy by Bone Regeneration with Deciduous Tooth Stem Cells, Dental Pulp Stem Cells, or Bone-Marrow-Derived Mesenc
Figures and illustrations from the paper.
Introduction
The purpose of studying bone-marrow-derived mesenchymal stem cells is to regenerate bone tissue using stem cells for dental implants. Bone defects lead to health problems which is the motivation behind this study. A challenge of dental implants is designing a biologically inert implant that will integrate into the surrounding tissue, which requires a sufficient amount of bone volume. The current gold standard is to use autogenous bone grafting, however bone grafts require injury to the organization of bone. Until recently, BMMSC and platelet-rich plasma have been studied for the purpose of regenerating bone. The purpose of this study is to regenerate the bone with minimal invasiveness using BMMSC in conjunction with other stem cells (dental pulp(DPSC), cells from human exfoliated deciduous teeth(DTSC) and MSCs) for dental implants.
Summary
The study used both human and canine models. The human dental pulp tissue was taken from deciduous teeth and permanent teeth. The human dental pulp stem cells and human deciduous tooth stem cells were cultured in low-glucose Dulbecco’s modified Eagle’s medium with 50 mL mesenchymal cell growth supplement, 10 mL of 200 mM L-glutamine and .5 mL penicillin-streptomycin containing 25 units penicillin and 25 micrograms streptomycin. The cells were incubated at 37 degrees Celsius in a humidified atmosphere.
The immunofluorescence analysis of STRO-1 for the human model was taken by first incubating with primary mouse anti-human STRO-1 antibody with a secondary goat anti-mouse IgM-FITC antibody. The cells were then incubated with various mouse antibodies to analyze the specific surface antigens. The cell fluorescence was evaluated using flow cytometry. RT-PCR analysis was conducted on days 7, 14, 21 and 28 of cultivation in the osteo-induction medium.
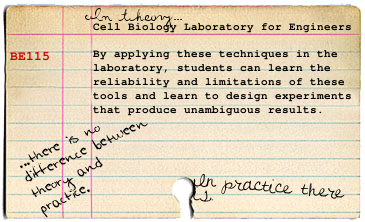
FIG. 1. (A) Cell morphology of human dental pulp stem cells (hDPSCs) (a) and human deciduous tooth stem cells (hDTSCs)
(d). Immunofluorescence staining of the stem cell marker STRO-1. hDPSCs (b) and hDTSCs (e) were positive for STRO-1 (green
fluorescence). DAPI was used to observe the nuclei (blue fluorescence). Alizarin red staining: hDPSCs (c) and hDTSCs (f). (B)
Typical flow cytometric analysis diagrams for expression of MSC markers CD13, CD29, CD44, and CD73, as well as hematopoietic
markers CD14 and CD34 antigens on hDPSCs (a–f) and hDTSCs (g–l). Unshaded peaks indicated negative control.
4
In the canine models, bone defects were implanted with graft materials: platelet-rich plasma, PRP plus canine bone marrow mesenchymal stem cells, PRP plus cDPSCs, and just the bone defect as the negative control. After 8 weeks, the implant was then inserted into the bone regenerated areas.
From the results of the RT-PCR analysis, the relative amounts of bone-related genes, ALP, Runx2 and OCN were measured in the human deciduous pulp stem cells and the deciduous tooth stem cells to see the osteogenesis potential. The results showed that the expression level of the genes increased compared to the conditioning medium which did not change.
FIG. 2. (A, B) Alkaline phosphatase (ALP), (C, D) Runx2, and (E, F) OCN gene expression levels in hDPSCs (A, C, E), and
hDTSCs (B, D, F) in the conditioning and induction medium. Control cells were cultured in the conditioning medium. On
days 7, 14, 21, and 28 of cultivation in the osteoinduction medium, cells were lysed for the extraction of total RNA. Equal
amounts of total RNA (50 ng) were analyzed by real-time reverse transcription–polymerase chain reaction, and the relative
expression levels of the ALP, Runx2, OCN, and glyceraldehyde OCN, Osteocalcin. 3-phophate dehydrogenase mRNAs in
each sample were quantitated by calculating their standard curves as described in the Materials and Methods section. The expression
coefficient for each mRNA on the ordinate was calculated by dividing the absolute level of expression of each mRNA
(ALP, Runx2, and OCN) with the absolute level of expression of glyceraldehyde 3-phophate dehydrogenase mRNA in each
sample in an attempt to compare the levels of gene expression quantitatively among different samples. Each point represents the
mean value calculated from five independent replicates, in which the difference was less than 10%. OCN, osteocalcin.
In the canine models, the stem cells were trypsinized at day 7 and were used for the implants. From the histological observations, cavities filled with the combination of PRP and stem cells resulted in new bone formation with a tubular pattern and abundant vascularization at 8 weeks. In the control and PRP sites, bone regeneration did not progress to allow dental implantation.
From this data, the researchers found that the stem cells from the pulp of permanent teeth and cells from exfoliated deciduous teeth appear to be an alternative and more readily available source of stem cells. The RT-PCR results were used to show that expression levels of ALP, OCN and Runx2 genes were enhanced in osteoblasts grown on coated implant surfaces. The results showed that cells differentiating into osteoblasts expressed higher levels of these genes than undifferentiated cells in the same medium which might show that the DPSCs and DTSCs might have the potential for bone regeneration. Also, the experimental results showed that in the control and PRP alone groups, the bone defect was surrounded by soft tissue that never healed and did not lend itself to implantation. In conclusion, the researchers note that DPSCs and DTSCs have several advantages over BMMSCs from other sources; the method of isolation was not invasive and they could be expanded rapidly in vitro.
Discussion
This paper was interesting as it tried to find an alternative source of stem cells to solve the problem of dental implants. The experiment seems to work pretty well as the use of canine DPSCs and canine DTSCs result in an increase in bone differentiating mRNA activity. As the actual trial was done in dogs, these findings may be limited to dogs. Also, it is unclear whether both types of stem deciduous stem cells work equally well. According to table 2, the peak of the expression coefficients occur at different times according to the type of stem cell used. It seems arbitrary to me why they chose to do RT-PCR analyses weekly.


7 comments:
Did they mention any strategies for scaling this up, to be of real use in potential therapies? It is an interesting alternative source, but it seems that unless they have a good way of increasing the stem cell population it is not so practical in a potential future clinical setting.
The potential of DPSCs and DTSCs for bone regeneration in dental implants is quite interesting. How were the cells implanted in the first place? Do you think that the addition of growth factors could improve the rate of bone regeneration?
@Luke The researchers suggest that one of the main advantages of the DPSCs and DTSCs is that the method of isolation is not invasive and can be expanded rapidly in vitro.
@Ed After culturing the cells, they were then implanted at the site of excision. As for the use of growth factors, the paper mentions reinforcemen of growth factor concentrations by application of the plasma rich platelets improves the bone regeneration and osseointegration.
I wonder how practical it would be to use these cells. Do the authors explain how they derived the human stem cells? If it's difficult to derive these cells from the patient, then there would probably be issues with the immune system if this method was tried with cells from random sources.
It'd be interesting to see if other papers in the literature have attempted to differentiate hESCs or iPS cells into the specific cell types needed to perform this kind of therapy.
Sorry, ignore my comment; I didn't read your previous response.
Anyways, I also wonder if culturing them in vitro has any effect on their function or differentiation state. I suppose this question is partly answered by their ability to differentiate into osteoblasts, but it'd be interesting to know to maximize the efficiency of the protocol.
Do you think the use of DTSCs and DPSCs is better suited for stabilizing the osseointegration of existing dental implants or could it be used for a more specific situation, that being the repair of existing teeth ie cavities? Could this even be done at all?
Are the RT-PCRs really comparable? The authors claim that there is no change in the control cultures, but I don't think that such a claim can be made without doing qRT-PCR. Also, did the authors explain why the mRNA concentrations appear to decrease at the latest time point? Though, again, this isn't quantitative at all. Also, the mRNA content doesn't increase for all cultures. Which cell line does each of the columns represent in the mRNA figure? Any explanation as to why the runx2 gene decreases over time?
Post a Comment